Information Current as of 11:00am EST on September 8, 2020.
North Carolina’s response to COVID-19 will continue to rapidly evolve. The most up to date information and guidance can be found at:
The respiratory disease named “coronavirus disease 2019” (abbreviated “COVID-19”), caused by a novel coronavirus named “SARS-CoV-2”, was declared a pandemic by the World Health Organization on March 11, 2020.
North Carolina now has community transmission of COVID-19. Therefore, we are moving to a different phase of our response efforts and will be further increasing our population-based community mitigation strategies. The goal of mitigation is to decrease spread of the virus among our population – especially for those who are at highest risk of clinical severity, and our health care workers – so fewer people need medical care at the same time. In addition, we need to implement strategies to conserve supplies and capacity so our health care workers can care for people who need medical attention even during the peak of the outbreak.
Appointments at Family Care
We have made a lot of changes to our scheduling and triage process over the last few months. Some changes you will notice include:
- When you arrive for your appointment, please stay in your car and call 919-544-6461 to check-in.
- We will screen you for possible COVID exposure over the phone and send a medical assistant to your car.
- Our medical assistant will check your temperature, sanitize your hands, and provide you with a mask, if you do not have one.
- More than 50% of our schedule is now done remotely, through phone consultations and telehealth (video chats).
- For med checks and visits that do not require a physical examination, we’ll try to arrange the visit remotely. This visit is structured similarly to a regular appointment, but saves you from unnecessary exposure to a medical office and helps with compliance to quarantine orders.
- Our schedules have been expanded to limit the number of patients physically present in our office at any time.
- More than 80% of our hours are now scheduled with only ONE patient in the office.
- The remaining times will still have only one patient for a provider visit, but another patient may also be getting lab work. These are done in separate, contained areas in the building.
- If you arrive early, you’ll need to wait in your car until your appointment time.
- If you need to complete paperwork, please call our office and we will bring it out to you to complete in your car.
Government Orders
- Governor Cooper’s September 1, 2020 Executive Order
- TLDR: Face masks are still required in public spaces.
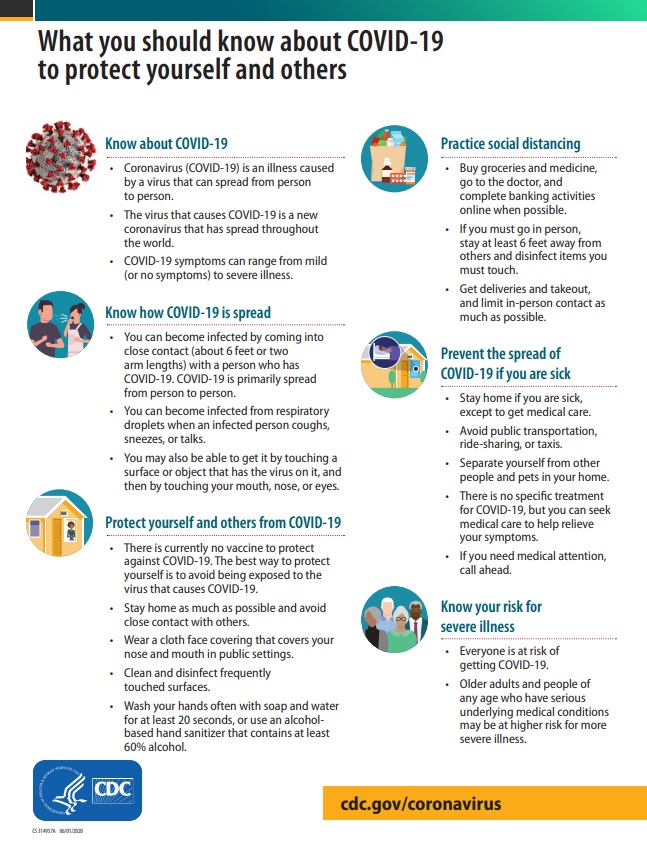
Know how COVID spreads
- There is currently no vaccine to prevent coronavirus disease 2019 (COVID-19).
- The best way to prevent illness is to avoid being exposed to this virus.
- The virus is thought to spread mainly from person-to-person.
- Between people who are in close contact with one another (within about 6 feet).
- Through respiratory droplets produced when an infected person coughs, sneezes or talks.
- These droplets can land in the mouths or noses of people who are nearby or possibly be inhaled into the lungs.
- Some recent studies have suggested that COVID-19 may be spread by people who are not showing symptoms.
Wash your hands often
- Wash your hands often with soap and water for at least 20 seconds especially after you have been in a public place, or after blowing your nose, coughing, or sneezing.
- It’s especially important to wash:
- Before eating or preparing food
- Before touching your face
- After using the restroom
- After leaving a public place
- After blowing your nose, coughing, or sneezing
- After handling your cloth face covering
- After changing a diaper
- After caring for someone sick
- After touching animals or pets
- If soap and water are not readily available, use a hand sanitizer that contains at least 60% alcohol. Cover all surfaces of your hands and rub them together until they feel dry.
- Avoid touching your eyes, nose, and mouth with unwashed hands.
Avoid close contact
- Inside your home: Avoid close contact with people who are sick.
- If possible, maintain 6 feet between the person who is sick and other household members.
- Outside your home: Put 6 feet of distance between yourself and people who don’t live in your household.
- Remember that some people without symptoms may be able to spread virus.
- Stay at least 6 feet (about 2 arms’ length) from other people.
- Keeping distance from others is especially important for people who are at higher risk of getting very sick.
Cover your mouth and nose with a cloth face cover when around others
- You could spread COVID-19 to others even if you do not feel sick.
- The cloth face cover is meant to protect other people in case you are infected.
- Everyone should wear a cloth face cover in public settings and when around people who don’t live in your household, especially when other social distancing measures are difficult to maintain.
- Cloth face coverings should not be placed on young children under age 2, anyone who has trouble breathing, or is unconscious, incapacitated or otherwise unable to remove the mask without assistance.
- Do NOT use a facemask meant for a healthcare worker. Currently, surgical masks and N95 respirators are critical supplies that should be reserved for healthcare workers and other first responders.
- Continue to keep about 6 feet between yourself and others. The cloth face cover is not a substitute for social distancing.
Cover coughs and sneezes
- Always cover your mouth and nose with a tissue when you cough or sneeze or use the inside of your elbow and do not spit.
- Throw used tissues in the trash.
- Immediately wash your hands with soap and water for at least 20 seconds. If soap and water are not readily available, clean your hands with a hand sanitizer that contains at least 60% alcohol.
Clean and disinfect
- Clean AND disinfect frequently touched surfaces daily. This includes tables, doorknobs, light switches, countertops, handles, desks, phones, keyboards, toilets, faucets, and sinks.
- If surfaces are dirty, clean them. Use detergent or soap and water prior to disinfection.
- Then, use a household disinfectant. Most common EPA-registered household disinfectantsexternal icon will work.
Monitor your health daily
- Be alert for symptoms. Watch for fever, cough, shortness of breath, or other symptoms of COVID-19.
- Especially important if you are running essential errands, going into the office or workplace, and in settings where it may be difficult to keep a physical distance of 6 feet.
- Take your temperature if symptoms develop.
- Don’t take your temperature within 30 minutes of exercising or after taking medications that could lower your temperature, like acetaminophen.
- Follow CDC guidance if symptoms develop.